Background : Tumor protein p53 ( TP53) mutations are associated with dismal outcomes in myelodysplastic neoplasms (MDS). However, the impact of TP53 allelic state in the context of allogeneic hematopoietic stem cell transplantation (allo-HSCT) for MDS has not been fully explored.
Method: We conducted a multi-center study in 347 MDS patients undergoing allo-HSCT between January 2017 and October 2022, with the median follow-up time among survivors of 28.6 (range, 4.7 - 76.6) months, and 45 had TP53 mutations among them.
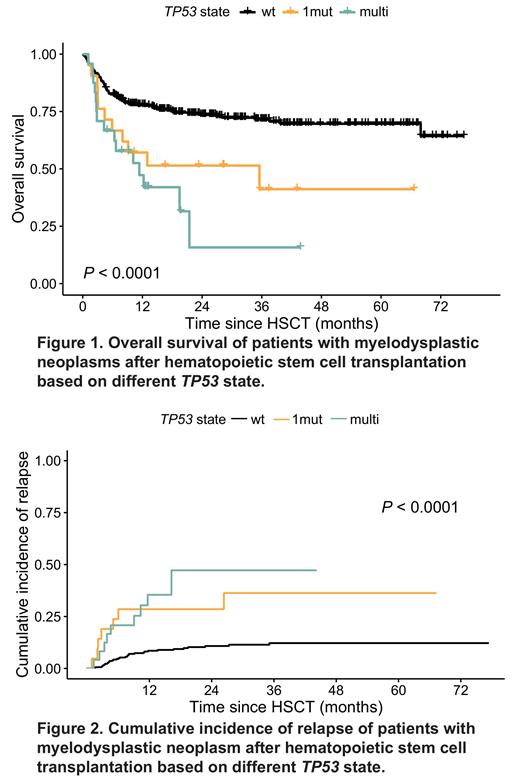
Results: Twenty-one patients were detected with TP53 monoallelic mutations ( TP531mut), while 24 had multiple hits ( TP53multi). Complex karyotype was more common in patients with mutated TP53 (52.4% of patients with TP531mutand 75.0% of patients with TP53multi), whereas this proportion was only 10.6% in patients with wild-type TP53 ( TP53wt). The prognosis varied according to different TP53 state, showing the 2-year overall survival (OS) rates of 51.4% (95% confidence interval [CI]: 33.7% - 78.6%) for TP531mut group versus 15.8% (95% CI: 3.3% - 76.4%) for TP53multi group versus 73.5% (95% CI: 68.5% - 78.9%) for TP53wt group ( P<0.001), and the 2-year cumulative incidence of relapse (CIR) rates of 28.6% (95% CI: 11.2% - 48.8%) for TP531mut group versus 47.3% (95% CI: 18.3% - 71.9%) for TP53multi group versus 10.8% (95% CI: 7.5% - 14.9%) for TP53wt group ( P<0.001). Similarly, the leukemia-free survival (LFS) and graft-versus-host disease-free/relapse-free survival (GRFS) of patients with TP531mut or TP53multi were obviously lower than those with TP53wt (both P<0.001). However, there was no significant difference on non-relapse mortality among these three groups ( P=0.424). The adverse effects of TP53 mutationson OS, LFS, GRFS and CIR were also found in patients undergoing haploidentical HSCT or those with molecular International Prognostic Scoring System high- and very high-risk categories (all P<0.05). In the subgroup with complex karyotype ( n = 32 with non-mutated TP53 and n = 29 with mutated TP53), significantly inferior OS, LFS and GFRS and higher CIR were observed in patients with mutated TP53 while in the subgroup without complex karyotype ( n = 270 with non-mutated TP53 and n = 16 with mutated TP53), there were no differences in these prognostic indicators (all P>0.05). Notably, among patients who received conventional conditioning regime without hypomethylating agents (HMA) ( n = 264 with non-mutated TP53 and n = 38 with mutated TP53), the inferior 2-year OS, LFS and GRFS rates, and the higher 2-year CIR rate of patients still presented in TP53 mutant patients(all P<0.05), but among those receiving conditioning regime containing HMA, similar outcomes were found between mutated ( n = 7) and non-mutated ( n = 38) TP53 groups (all P>0.05). Multivariable cox proportional hazards models demonstrated that monoallelic TP53 state was an independent risk factor for survival and relapse (HR OS=2.859, 95% CI: 1.372 - 5.957, P=0.005; HR LFS=2.566, 95% CI: 1.342 - 4.905, P=0.004; HR GRFS=2.146, 95% CI: 1.106 - 4.163, P=0.024; HR CIR=2.507, 95% CI: 1.033 - 6.086, P=0.042), and multi-hit TP53 state also predicted worse outcomes (HR OS=3.038, 95% CI: 1.453 - 6.356, P=0.003; HR LFS=2.716, 95% CI: 1.383 - 5.336, P=0.004; HR GRFS=1.882, 95% CI: 1.002 - 3.535, P=0.049).
C onclusions: Monoallelic and multi-hit TP53 state identify a high-risk group for poor outcomes in MDS patients undergoing allo-HSCT, complex karyotype could amplify the adverse prognostic effect of TP53, and these patients might benefit from receiving conditioning regime containing HMA.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal